THE ECHOCARDIOGRAM
The echocardiogram is an extremely useful test for studying the heart’s anatomy. It is a non-invasive and entirely safe, and when interpreted by well-trained cardiologists, is very accurate.
The patient lies on a bed or examination table, and the echo technician places a transducer (a device that resembles a computer mouse) over the chest wall. The transducer is moved back and forth across the chest wall, collecting several “views” of the heart.
The transducer placed on the chest sends sound waves toward the heart. Like the sonar on a submarine, the sound waves bounce off the cardiac structures (that is, they echo: off the heart). The sound waves “echos” are collected by the transducer.
These returning sound waves are computer processed, and a two dimensional image of the beating heart is produced on a television screen.
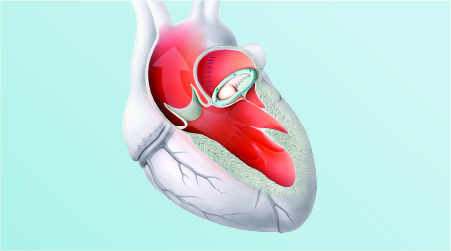
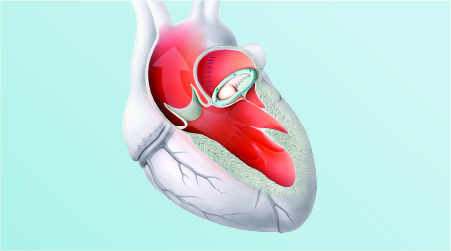
What is Ejection Fraction (EF)?
Your heart circulates blood through 2 separate systems. The two chambers on top (atriums) are receiving stations for blood. The two lower chambers (ventricles) are pumping stations. Your left ventricle forces oxygen-rich blood into your arteries, which carry it throughout your body. The blood returns to the right atrium, which passes it down to the right ventricle. The right ventricle pumps this blood to the lungs, where it picks up oxygen. Oxygen rich blood then returns to the left atrium, which dumps it into the left ventricle, and the cycle repeats. Valves between the chambers prevent “backwash”.
When the left ventricles contracts, forcing blood out into the body, it is called “ejection” since it is “ejecting” the blood out into your arteries. Since the big pump on the lower left is the one that pushes blood throughout your body, that is where they usually measure heart function – the left ventricle.
That’s the “fraction” part. The “fraction” part is because that pumping chamber never quite manages to pump out all the blood inside it – there’s always a little bit left behind that lies around waiting for the next contraction. The amount your left ventricle does pump out beat is called the “ejection fraction”. It’s X% (the amount pumped out) of the total amount of blood in the ventricle per heart beat.
THE EXERCISE STRESS TEST
Some forms of cardiac disease are easily missed when the patient is at rest, because at rest the patient’s physical examination and ECG are often entirely normal. In these cases, cardiac abnormalities may become apparent only when the heart is asked to perform at increased workloads.
The stress test is used to evaluate the heart and vascular system during exercise. It helps to answer two general questions
1. Is there occult underlying heart disease that only becomes apparent when the heart is stressed by exercise?
2. If there is underlying heart disease, how severe is it?
How is a stress test performed ?
The patient is attached to an ECG machine, and a blood pressure cuff is placed on one arm. Sometimes a clothespin-like sensor is attached to the finger to measure the amount of oxygen in the blood. After a baseline ECG is obtained, the patient begins to perform a low level of exercise, either by walking on a treadmill, or pedaling a stationary bicycle. The exercise is “graded” – that is, every three minutes, the level of exercise is increased. At such “stage” of exercise, the pulse, blood pressure and ECG are recorded, along with any symptoms the patient may be experiencing.
With a “maximal” stress test, the level of exercise is gradually increased until the patient cannot keep up any longer because of fatigue, or until symptoms (chest pain, shortness of breath, or lightheadedness) prevent further exercise, or until changes on the ECG indicate a cardiac problem. Maximal stress test should be performed when the goal is to diagnose the presence or absence of coronary artery disease.
With a “sub maximal” stress test, the patient exercise only until a pre-determined level of exercise is attained. These tests are used in patients with known coronary artery disease, to measure whether a specific level of exercise can be performed safely.
After the test, the patient remains monitored until any symptoms disappear, and until the pulse, blood pressure and ECG return to baseline. This test is also popularly called TMT or Trade Mill Test.
What are the risks of having a stress test ?
The stress test has proven to be remarkably safe. It poses about the same level of risk as taking a brisk walk or walking up a hill. While it is possible that the ischemia provoked by such stress can lead to a myocardial infarction (heart attack) or to serious heart rhythm disturbances, in practice this event is rare. Further, when these serious events do occur during a stress test, they occur in the presence of trained medical personnel who can deal with them immediately.

CT ANGIOGRAPHY
It is the latest non-invasive test which has created a lot of hope for the heart patient. This is a simple test, there is no admission required. You just lie down on the table, one injection will be given and the table moves in such a way that your chest is inside a round circle. The scan now takes about one minute and the test is over. CT angiography will be able to tell your level of blockage and where they are situated. This test is little expensive (about Rs.6000 to 15000) but is almost as accurate as the catheter angiography. This test can be repeated after one or two years to know the reversal of the blockages. This test has come to India only few years back and many people are not aware of this test. Till now the machines are available only in metro cities. This is one of tests which have no side effects and Saaol recommends this test to many. This test has created a major problem for the heart hospital cardiologists as it competes with their own catheter angiography.
The major reason is that the patient comes to know of the blockages without admission in the hospital and they cannot be pressurized for the angiography and the bypass surgery. Usually, after the catheter angiography, the cardiologists prevail upon the admitted patients; put pressure on them and the relatives and make them agree for such treatments which give lot of money. On public demand many hospitals have installed this machine as more people want to know about their condition from outside. But you talk to the cardiologists in the same hospital; they will not encourage you to undertake this test.
.

CORONARY ANGIOGRAPHY (NOT AN ORDINARY TEST) – INVASIVE TEST
Coronary Angiography is an X-ray examination of the blood vessels of the heart. A tube is inserted in your groin. The tube is now blindly passed into the body from outside. When positioned either in the heart or at the beginning of the arteries supplying the heart, a special fluid (called a contrast medium or dye) is injected. This fluid is visible by X-ray and the pictures that are obtained are called angiograms.
Coronary Angiography is not an ordinary test. It is an invasive procedure where a foreign body in the form of catheter is inserted inside the body through a cut. This carries a lot of risk. Following can occur during or after the procedure.
Death: Certain patient groups are at increased risk of death during the angiography. They can be elderly above 60 years, patients with angina class IV, those with blockages in the left main coronary artery. Also patients with previous heart attacks and low cardiac function, with valvular heart diseases or with non-cardiac disease like kidney disease, diabetes (IDDM) etc are at risk.
Heart Attack or Myocardial Infarction: The wire can cause an injury to the intima (inner covering of blood tubes) leading to formation of a blood clot and eventually a heart attack. Patients with excessive blockages or blockages in left main with IDDM having angina at rest are more prone for heart attack.
Brain Injury: The blood clots as described above can move to the arteries of the brain which can lead to brain stroke (paralysis). Delayed hemorrhage (bleeding) is also on =e of the complications. The collection of blood can compress nerves and other blood tubes. This can cause severe brain injury.
Injury or puncture of the blood tubes: The wire after inserting and moving towards the heart can puncture any blood tube through which it passenos. It can also move into blood tubes of other organs like the kidney’s, legs etc. and cause injury. This, in turn, can result in internal haemorrhage and organ damage. In this manner, the heart tubes can be punctured. The scratches in the blood tubes during the procedure caused by the wire always help in more deposition of cholesterol and triglycerides and hence development of new blockages.
Arrhythmias (disturbances in the normal rhythm of the heart): The normal beating of the heart can be disturbed and may result beats or reduced heartbeats. Also the pattern of heart contraction may be damaged. Cardiac Arrest or Cardio-genic shock: The vasovagal reaction can lead to cardiac arrest or shock. Infection, fever: The wire introduced is a foreign body. It can lead to infection inside the blood tubes and create further complications. Reactions can also results by contaminating materials that may remain on incompletely cleaned wire surfaces.
 Allergies and Anaphylaxis (severe reactions): The local anaesthesia and the dye used can cause severe allergic reactions which can even cause death.
Allergies and Anaphylaxis (severe reactions): The local anaesthesia and the dye used can cause severe allergic reactions which can even cause death.
Hypotension: The reactions mentioned above can result in lowering of blood pressure. This can lead to damage to other organs. It can also cause kidney damage, bleeding lungs and respiratory insufficiency.
Result of Angiography – Is it accurate ?
If you notice, most of the blockages are reported as 70%, 80%, or 90%. Why these round figures? Some write 75%, 85% or 95%. The results are only a visual estimation. The figures often change by 10-20%, if you take an independent opinion from cardiologists. The surgeons have a tendency to increase all the blocks and the angioplasty doctors enhance one blockage but reduce the figure of others. The bias is to benefit themselves. If the results were accurate the figures would have been 71.7% or 92.5%.
Specialized tests for the heart
These tests are only used in few of the patients where it is specially indicated. They are:
1. Stress Thallium Test/Nuclear Perfusion tests
2. PET scan
3. MRI Scan
4. Cardiac MRI test
5. Holter Test
6. EPS or Electrophysiological Study
If you want to read about them read the annexure called Specialized heart's tests

Specialized tests for the heart
These tests are only used in few of the patients where it is specially indicated. They are:
1. Stress Thallium Test/Nuclear Perfusion tests
2. PET scan
3. MRI Scan
4. Cardiac MRI test
5. Holter Test
6. EPS or Electrophysiological Study
STRESS THALLIUM SCAN – THE NUCLEAR PERFUSION STUDY
The thallium scans are tests that show how well blood is flowing to various portions of the heart muscle. These tests, which are varieties of nuclear perfusion studies, are generally used in conjunction with stress tests to non-invasively diagnose the presence of coronary artery disease. Thallium is a radioactive substance. When injected into the bloodstream, this collects in the portions of heart muscle that have good blood flow. If one of the coronary arteries (the arteries that supply blood to the heart muscle) is blocked or partially blocked, not as much thallium accumulates in the muscle supplied by that blocked artery.
How is nuclear perfusion studies performed ?
During a stress test, thallium is injected into the patient’s vein when the maximum level of exercise is reached. The radioactive substance distributes itself throughout the cardiac muscle in proportion to the blood flow received by that muscle. Cardiac muscle receiving normal blood flow accumulates the larger amount of thallium than cardiac muscle that is supplied by diseased coronary arteries. An image of the heart is then made by a special camera that can “see” the thallium. From these pictures, portions of the heart that are not receiving normal blood flow (because of blockages in the coronary arteries) can be identified.
Using thallium perfusion imaging greatly increases the accuracy of the stress test in diagnosing coronary artery disease. A normal thallium test is an excellent indication that the patient has no significant coronary artery disease. Patients with abnormal perfusion scans are likely to have significant coronary artery disease. These non-invasive studies are very safe. Their only drawback is that radiation is used – but the patient is exposed only to about the same amount of radiation as for a chest x-ray.
WHAT IS A PET SCAN ?
PET stands for Positron Emission Tomography. That fact in itself is amazing, because it means that through research, man has predicted the existence of, discovered and is now using anti-matter (a positron is the anti matter equivalent of an electron). A PET scan uses a small dosage of a chemical called radionuclide combined with a sugar. This combination is injected to into patient. The radionuclide emits positrons. A PET scanner will rotate around a patient’s head to detect the positron emissions given off by the radionuclide. Because malignant tumors are growing at such a fast rate compared to healthy tissue, the tumor cells will use up more of the sugar which has the radionuclide attached to it. The computer then uses the measurements of glucose used to produce a picture which is color coded.
Heart Disease: How Can a PET Make a Difference ?
PET scans of the heart allow the study and qualification of various aspects of heart tissue function. Clinical studies show an important role for PET in diagnosing patients, describing disease and developing treatment strategy. Two areas of clinical application have emerged:
PET is the most accurate test to reveal coronary artery disease and impaired blood flow or rule out its presence. PET is the gold standard to determine the viability of heart tissue for revascularization.
PET can determine whether bypass surgery or transplant is the appropriate treatment. PET provides a way to assess the severity of heart disease and measure its impact on heart function.
The heart has a unique way of providing increased blood flow that is needed during period of exercise or stress. A network of collapsed arteries or veins, called flow reserve, is ready to be used if the heart needs it. The heart also has the ability to develop collateral vessels to bring blood to heart tissues that may need more. When narrowing of the vessels occur with coronary heart disease, some of these collapsed vessels open, so the heart can maintain optimal flow.
A portion of the flow that should be reserved for stress or exercise is needed for resting function. In fact, blood flow to the heart tissue at rest is not decreased (so that symptoms may not be detected) until the blockage is extensive, which may be when all the collapsed vessels in the area are fully is use to address the needs of the heart at rest. Further narrowing or blockage prevents the heart muscle from getting the blood it needs, even at rest.
CARDIAC MAGNETIC RESONANCE IMAGING (MRI)
These techniques take detailed anatomic pictures of the body. The pictures are acquired by exposing the body to magnetic fields. This causes energy to be released by hydrogen atoms in the body. This emitted energy is detected and the picture of the interior of the body is constructed. Side effects are rare and mild. Sometimes, an intravenous injection of something called gadolinium is also given.
Traditional magnetic resonance imaging (MRI) scanners require that the patient be placed in a small cylindrical tube. This can be somewhat unsetting for claustrophobic patients. Newer scanners are more open but do not produce the high quality pictures that the closed scanners do. Patients can expect to hear loud knocking noises from the scanner as the images are required. Because of the powerful magnets used, patients with pacemakers or certain other metallic substances in their body cannot undergo this procedure. Note that patients with some types of metal, such as artificial heart valves and artificial hips, can undergo this procedure safely. It is important to let the staff of the MRI unit know the patient’s complete medical history so that they can determine if the procedure can be safely performed.
In cardiology, MRI scans are primarily used to evaluate the aorta (the main blood vessels that supplies blood to the rest of the body). The chambers of the heart and the strength of the heart muscle can be visualized. Leaky and narrowed heart valves can be evaluated. Tumors in the heart can be detected. MRI is an excellent test to assess congenital heart disease. Stress tests can be performed with MRI also. Much of the same information can be obtained more conveniently and at lower cost by standard echo-cardiography or transesophageal cardiography. However, there are rare situations when MRI scanning is required.
Magnetic Resonance Angiography (MRA) is an MRI scan that essentially produces an angiogram, i.e. pictures of the blood vessels. It is quite useful for larger blood vessels such as the aorta and the arteries that go to the brain. It is getting better as time goes on for picturing the small, curving coronary arteries that lie on the surface of the beating heart. It holds promise for the future.

HOLTER MONITORS AND EVENT RECORDERS (AMBULATORY MONITORING)
Ambulatory Monitoring (holter monitoring and event recorders) is done to record a patient’s ECG for a prolonged period of time, on an outpatient basis. The purpose of ambulatory monitoring is to look for evidence of cardiac transient problems-i.e. problems that come and go, that are not apparent when a standard ECG is performed. Ambulatory monitoring is particularly useful in diagnosing transient heart arrhythmias, and transient cardiac ischemia.
How is Ambulatory Monitoring performed?
There are two general types of ambulatory monitoring – the Holter monitor and the Event recorder. With the Holter monitor, electrode leads are applied to the skin (similar to the leads used in recording a standard ECG), and attached to a tape recorder. The patient is sent home and resumes normal activities while the tape recorder records a continuous ECG tracing for 24 or 48 hours. The Holter equipment is then removed, and the tape is analyzed.
In contrast, event recorders do not record every heart beat on a tape. Instead, event recorders use a circular tape that stores only approximately 30 seconds of a patient’s heart rhythm. That is, at any given time while a patient is wearing them, event recorders will have the most recent 30 seconds of the patient’s ECG. When the patient experiences the symptom of interest, he/she presses a button that freezes the recording, which is then transmitted by telephone to an interpreting center. A major advantage of event recorders is that they can be used for up to 30-60 days, until the transient symptom being looked for occurs. Another advantage is that, as long as the symptom of interest typically lasts for more than a minute or two, the ECG electrodes do not actually need to be attached all the time. Since attaching the electrodes takes less than a minute, they can simply attach as needed.
EPS Study
An electrophysiology (EP) study is a test performed to assess your heart's electrical system or activity and is used to diagnose abnormal heartbeats or arrhythmia. The test is performed by inserting catheters and then wire electrodes, which measure electrical activity, through blood vessels that enter the heart.
The Procedure
The EP study is performed in the electrophysiology laboratory of the hospital, where you'll be placed on an X-ray table. A camera and television screens, heart monitors and various instruments will be close by. Electrodes will be placed on your chest and back to connect you to monitoring equipment. A blood pressure cuff will be placed on your upper arm to monitor your blood pressure.
To prevent infection, a nurse will shave and cleanse the groin and possibly neck area where the catheters will be inserted. The area will be cleansed with an antiseptic. Sterile sheets will be draped over your body. Find a comfortable position so you can remain still during the procedure. Please don't touch the sterile areas on your neck and groin.
Depending on the type of study you undergo, you may be given medications intravenously, administered in your arm, to sedate you or make you sleepy. These medications help reduce your anxiety and relieve your discomfort. Your doctor will let you know if sedation medications are appropriate.
A local anesthetic will be administered with a tiny needle to numb the area where the catheters are inserted. You will feel a pinprick and possibly a stinging sensation for a few seconds. One or more catheters, which are thin, long, flexible wires, will be inserted into a large vein in your groin or neck. The catheters will be guided to your heart. The positioning of catheters inside your heart will be monitored on a screen. You may feel pressure when the catheters are inserted. The incision site is less than a quarter of an inch.
There are two parts to the EP study
Recording the heart's electrical signals to assess the electrical function
Pacing the heart to bring on certain abnormal rhythms for observation under controlled conditions Medications are sometimes used to stimulate your arrhythmia. You may feel your heart racing or pounding. This may make you anxious, but you needn't be alarmed. The doctors want to induce the abnormal rhythm causing your problem, so they can treat the arrhythmia. If you have any uncomfortable symptoms — such as chest pain, dizziness, shortness of breath, nausea and pain.
What are the risks of EPS ?
Risks may include
Arrhythmia. During EPS you may have abnormal heart rhythms that make you dizzy. If this happens, your doctor may give your heart an electric shock to bring back a regular heartbeat.
Blood clots sometimes can form at the tip of the catheter, break off and block a blood vessel. Your doctor may give you medicine to prevent blood clots.
Infection, bleeding and bruising at the site where the catheter went in (groin, arm or neck). Your doctor or nurse will help you avoid these problems.

 India
India